In the modern dental practice, diagnostic imaging is an indispensable tool, offering invaluable insights into oral health. From detecting caries to planning complex restorative procedures, X-rays play a critical role in providing comprehensive patient care. Yet, with the benefits of radiographic imaging comes the inherent responsibility to manage radiation exposure meticulously. Ensuring the safety of both patients and staff from unnecessary radiation is not just a regulatory requirement; it’s a cornerstone of ethical practice and patient trust. This is where a well-structured framework, such as a Dental Radiation Protection Program Template, becomes an essential asset for any dental office.
A robust radiation protection program isn’t merely a document to satisfy an inspector; it’s a living guide that permeates every aspect of your practice’s imaging protocols. It provides clear guidelines, fosters a culture of safety, and demonstrates an unwavering commitment to patient and employee well-being. For busy dental professionals, developing such a comprehensive program from scratch can be a daunting task. This is precisely why a thoughtfully designed template offers an invaluable starting point, streamlining the process of establishing and maintaining exemplary radiation safety standards.
The Unseen Imperative: Why Radiation Safety is Non-Negotiable
Understanding the "why" behind radiation safety protocols is fundamental to effective implementation. Ionizing radiation, while beneficial for diagnostic purposes, carries the potential for biological effects on living tissue. While modern dental X-ray units are designed for minimal exposure, and the doses are typically very low, the principle of "as low as reasonably achievable" (ALARA) remains paramount. This principle guides all aspects of a radiological protection plan, striving to minimize exposure without compromising diagnostic quality.
Beyond the ethical imperative to protect patients and staff, dental practices in the United States operate under a complex web of federal and state regulations. These regulations mandate specific requirements for X-ray equipment, operator qualifications, safety procedures, and documentation. Failure to comply can lead to significant penalties, legal repercussions, and damage to a practice’s reputation. A comprehensive radiation safety program serves as your primary defense, ensuring that your practice not only meets but often exceeds these baseline requirements, fostering a truly safe environment.
Building Your Shield: Core Components of a Robust Program
A highly effective radiological protection program is multifaceted, addressing various aspects of a practice’s operations. It should be dynamic, clear, and easily accessible to all relevant personnel. Here are the fundamental components every dental office should integrate into its safety framework.
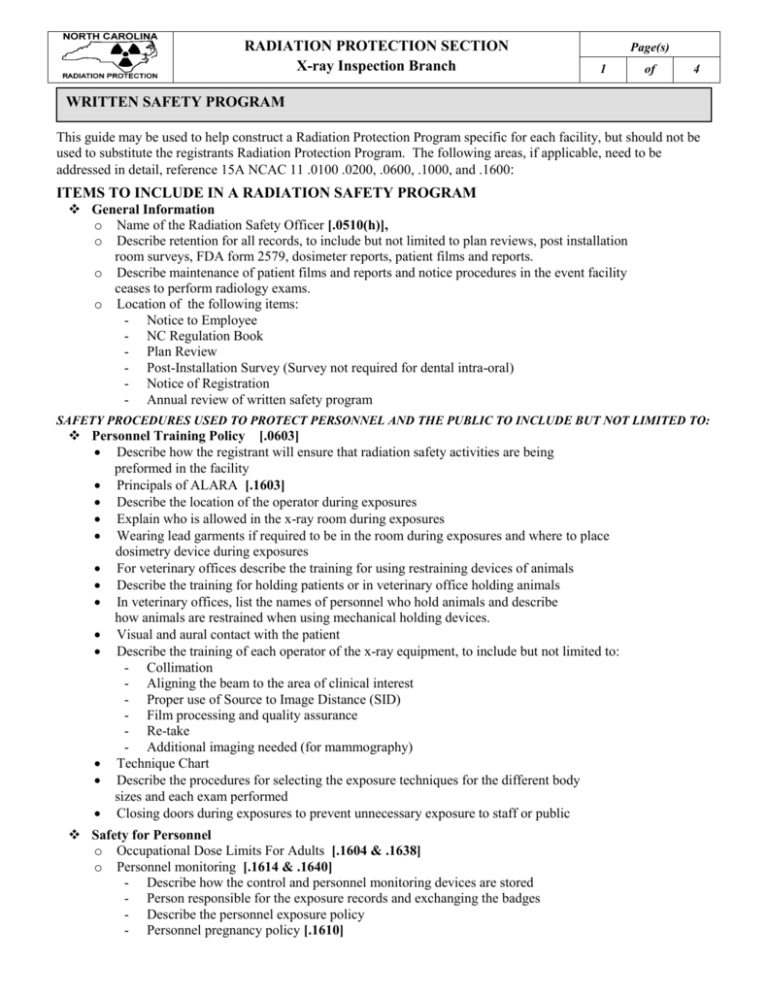
Administrative Controls
Effective administration forms the backbone of any successful safety initiative. These controls define roles, responsibilities, and the overarching policies that govern radiation use within the practice.
- Designation of a **Radiation Safety Officer (RSO)** or equivalent, responsible for overseeing the program.
- Clear **policy statements** outlining the practice’s commitment to radiation safety and the ALARA principle.
- Protocols for **incident reporting** and investigation in case of equipment malfunction or accidental overexposure.
- Maintenance of comprehensive **documentation** including equipment logs, staff training records, and patient exposure histories.
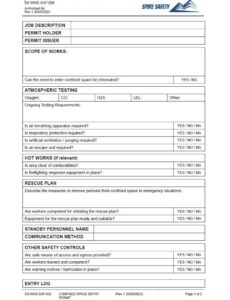
Operational Protocols
These are the day-to-day procedures that ensure safe and effective use of X-ray equipment. They cover the practical steps taken during every radiographic procedure.
This includes detailed instructions for patient positioning, selection of appropriate exposure settings based on patient size and diagnostic need, and the proper use of protective barriers. Emphasis is placed on minimizing retakes through meticulous technique and strict adherence to established guidelines. The goal is to obtain the highest quality diagnostic image with the lowest possible radiation dose, every single time.
Patient Protection Measures
Protecting patients from unnecessary radiation exposure is a primary concern. Several key strategies are employed to achieve this goal.
The use of lead aprons and thyroid collars is standard practice, shielding sensitive organs from scatter radiation. Image receptor selection also plays a crucial role; digital sensors and high-speed films significantly reduce exposure times compared to older technologies. Furthermore, strict criteria for radiographic examination selection, avoiding routine or unnecessary X-rays, are paramount. Radiographs should only be taken when there is a clear diagnostic need, based on clinical assessment and patient history.
Staff Training and Monitoring
A well-informed team is crucial for maintaining a high standard of radiation safety. Comprehensive training ensures that all personnel involved in radiography understand the risks and proper safety protocols.
Initial training for new staff covers basic radiation physics, biological effects, regulatory requirements, and practice-specific procedures. Ongoing education and refresher courses are essential to keep staff updated on new technologies, revised guidelines, and best practices. For staff members who frequently operate X-ray equipment, individual dose monitoring, often through dosimeter badges, provides an objective measure of occupational exposure, ensuring it remains well within safe limits.
Equipment Maintenance and Quality Assurance
The reliability and accuracy of X-ray equipment directly impact radiation safety. Regular maintenance and stringent quality assurance (QA) protocols are non-negotiable.
Routine equipment checks, calibration, and preventative maintenance by qualified technicians ensure that units are functioning optimally, preventing unnecessary radiation leakage or inaccurate doses. QA programs include daily, weekly, and monthly tests of X-ray units, processing equipment, and digital sensors to ensure consistent image quality and proper operation. This proactive approach minimizes errors and maximizes the diagnostic utility of every exposure.
Leveraging a Program Framework for Success
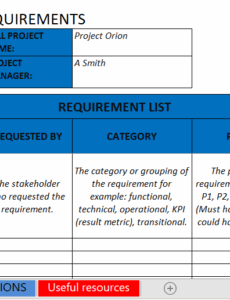
Adopting a pre-structured framework, like a Dental Radiation Protection Program Template, offers significant advantages over building one from the ground up. It provides a comprehensive outline that incorporates industry best practices and regulatory requirements, saving countless hours of research and writing. This efficiency allows dental professionals to focus more on patient care and less on administrative burdens.
Streamlining Compliance
Navigating the myriad of state and federal regulations concerning radiation safety can be complex. A well-designed program framework acts as a checklist and a guide, ensuring that your practice addresses all mandated elements. It simplifies the process of demonstrating compliance during inspections and helps to avoid potential oversights that could lead to non-compliance issues. This organized approach brings peace of mind, knowing your practice is consistently meeting its legal and ethical obligations.
Ensuring Consistent Best Practices
A standardized radiological protection plan ensures that every team member follows the same established procedures for radiography. This consistency reduces variability in technique, minimizes errors, and guarantees that every patient receives the same high level of care and protection. It fosters a predictable and safe environment, regardless of which team member is operating the X-ray equipment. This uniformity is vital for maintaining quality control and preventing preventable incidents.
Facilitating Staff Education
An existing framework provides a clear, organized resource for staff training and onboarding. New employees can quickly grasp the practice’s radiation safety protocols, and existing staff can easily review procedures and stay updated. This accessibility enhances the overall safety culture within the practice, empowering every team member to be an active participant in maintaining a safe environment. It also serves as an excellent reference manual for any questions that may arise regarding specific protocols.
Beyond the Basics: Customization and Continuous Improvement
While a template provides an excellent foundation, it’s crucial to remember that it is a starting point, not a final solution. Every dental practice has unique characteristics: different equipment, varying patient demographics, and distinct operational workflows. Therefore, customizing the program to fit your specific needs is essential. This involves reviewing each section of the template and tailoring it with your practice’s specific policies, equipment details, and assigned responsibilities.
The process of radiation protection is not static; it requires continuous improvement. Regularly review your radiological protection program, at least annually, or whenever there are significant changes in equipment, personnel, or regulations. Gather feedback from your team, conduct drills, and analyze any incidents or near misses to identify areas for enhancement. Fostering a culture of safety means embracing a mindset of vigilance and adaptation, always striving to achieve the highest possible standards for patient and staff protection.
Implementing a comprehensive radiation protection program is a clear demonstration of your practice’s commitment to safety, quality, and ethical patient care. It is an investment in your team’s well-being, your patients’ trust, and the long-term success and reputation of your practice. By utilizing a robust template and dedicating time to its customization and ongoing refinement, you can establish a framework that not only meets regulatory demands but also elevates your standard of care, ensuring a safe and secure environment for everyone. This proactive approach is a hallmark of dental excellence, building confidence and fostering a reputation for uncompromising safety.