In an increasingly digital world, the healthcare sector stands at a critical juncture, navigating the twin demands of efficiency and stringent regulatory compliance. The days of endless paper trails, manual signatures, and cumbersome physical storage are rapidly giving way to streamlined digital processes. Central to this transformation is the adoption of electronic signatures, a technology that promises to revolutionize how healthcare providers manage everything from patient consent forms to internal HR documents and administrative agreements.
However, simply adopting electronic signature technology isn’t enough; a robust framework is required to ensure its proper, secure, and legally compliant use. This is where an Electronic Signature Policy Template For Healthcare becomes indispensable. It serves as a foundational guide for organizations looking to formalize their digital signing practices, ensuring consistency, security, and adherence to crucial regulations like HIPAA. For healthcare administrators, compliance officers, IT managers, and legal teams, understanding and implementing such a template is not just about keeping pace with technology, but about safeguarding patient data, improving operational workflows, and mitigating significant legal risks.
Why an Electronic Signature Policy Template For Healthcare is Essential
The modern healthcare landscape is defined by rapid technological advancement and ever-evolving regulatory demands. In this environment, the judicious use of electronic signatures is no longer a luxury but a necessity. An Electronic Signature Policy Template For Healthcare provides the much-needed framework to navigate this complexity.
Firstly, it addresses the critical need for compliance with federal and state regulations, most notably the Health Insurance Portability and Accountability Act (HIPAA) in the United States. HIPAA mandates strict privacy and security standards for protected health information (PHI). An effective policy ensures that electronic signatures are implemented in a manner that protects data integrity and patient privacy, establishing secure workflows for obtaining patient consent, managing treatment plans, and handling billing agreements. Without a clear policy, organizations risk significant penalties for non-compliance.
Secondly, the shift towards electronic health records (EHRs) and telehealth services has amplified the volume of digital documents requiring authentication. Whether it’s a doctor signing off on a prescription, a patient consenting to a procedure, or an employee acknowledging a new HR policy, electronic signatures accelerate these processes. A well-defined Electronic Signature Policy Template For Healthcare ensures that all these digital interactions are legally sound and trustworthy, providing non-repudiation and clear audit trails for every transaction. This level of accountability is vital for both clinical and administrative oversight, safeguarding the organization against potential disputes or legal challenges.
Key Benefits of Using an Electronic Signature Policy Template For Healthcare
Implementing a comprehensive Electronic Signature Policy Template For Healthcare yields a multitude of advantages that impact every facet of a healthcare organization. These benefits extend beyond mere digital convenience, touching upon operational efficiency, cost savings, enhanced security, and improved patient experience.
One of the most immediate benefits is enhanced operational efficiency and workflow optimization. By replacing manual, paper-based signing processes, healthcare providers can drastically reduce administrative burdens. Documents can be signed and routed instantly, accelerating patient intake, consent management, and approval processes for internal administrative documents. This frees up staff to focus on patient care rather than paperwork.
Significant cost savings are another compelling advantage. Eliminating the need for printing, scanning, mailing, and physical storage of paper documents translates into substantial reductions in material costs, storage space, and staff time previously dedicated to managing paper. An Electronic Signature Policy Template For Healthcare helps realize these savings by formalizing the digital transition.
Furthermore, a robust policy bolsters security and data integrity. Electronic signatures, when implemented correctly with appropriate encryption and authentication protocols, are often more secure than their wet-ink counterparts. The policy outlines requirements for secure digital certificates, multi-factor authentication, and robust audit trails, making it far more difficult to tamper with documents or forge signatures. This level of data security is paramount for sensitive patient information.
Finally, integrating a standardized Electronic Signature Policy Template For Healthcare improves patient and staff experience. Patients benefit from a streamlined, often remote, signing process that is more convenient and less time-consuming. Staff members appreciate the reduction in manual tasks and the ease of accessing digitally signed documents, contributing to a more efficient and less stressful work environment. It also supports the increasing demand for digital accessibility and a paperless environment.
Customizing and Adapting Your Electronic Signature Policy Template For Healthcare
While an Electronic Signature Policy Template For Healthcare provides an excellent foundation, its true value is unlocked through careful customization and adaptation to fit the unique context of your organization. Healthcare environments vary widely, from small, single-provider clinics to sprawling multi-specialty hospital systems, each with distinct operational models, technological infrastructure, and patient demographics.
For smaller practices, customization might focus on simplicity and ease of integration with existing practice management software or basic EHR systems. The policy should be straightforward, clearly defining user roles and basic security protocols, and perhaps utilizing readily available, user-friendly e-signature platforms. The goal is to ensure quick adoption without overwhelming staff with overly complex compliance requirements that might be more relevant to larger entities.
Conversely, large hospital networks or integrated delivery systems will require a more comprehensive and granular Electronic Signature Policy Template For Healthcare. This could involve detailed sections on enterprise-wide system integrations, specific departmental procedures (e.g., for admissions, billing, HR, pharmacy, clinical documentation), disaster recovery protocols, and advanced audit capabilities. These organizations often deal with a higher volume of diverse document types and a broader range of users, necessitating robust governance and scalability built into the policy.
Furthermore, adapting the template involves considering specific legal and regulatory nuances of the states in which you operate. While federal laws like ESIGN and UETA provide a national framework, some states may have additional requirements for certain types of documents or specific industries. Collaboration with legal counsel is crucial during this customization phase to ensure the policy reflects all applicable regulatory requirements. The policy should also be flexible enough to accommodate future technological advancements and evolving best practices in data security and digital transformation.
Important Elements to Include in Your Electronic Signature Policy Template For Healthcare
A comprehensive Electronic Signature Policy Template For Healthcare must address several critical components to ensure legal enforceability, security, and operational integrity. Omitting any of these elements could expose the organization to risks.
Here are the key elements that should be included:
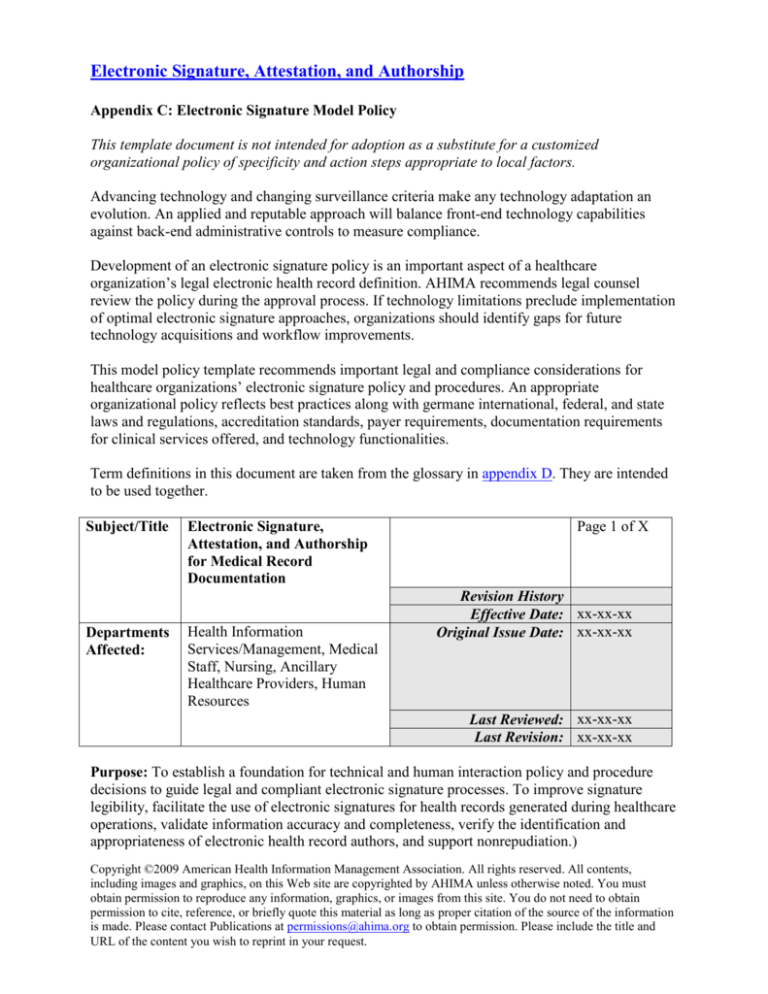
- Policy Statement and Purpose: Clearly articulate the policy’s objective, which is typically to govern the creation, use, and acceptance of electronic signatures within the organization, ensuring compliance with relevant laws and regulations.
- Scope and Applicability: Define who the policy applies to (all employees, contractors, third-party partners) and what types of documents and transactions it covers (patient records, HR documents, financial agreements, consent forms).
- Definitions: Provide clear, unambiguous definitions for key terms such as "electronic signature," "digital signature," "signer," "document custodian," "audit trail," and "protected health information (PHI)."
- Legal Basis and Compliance: Explicitly state the legal frameworks that underpin the policy, including the ESIGN Act, UETA (Uniform Electronic Transactions Act), HIPAA, and any relevant state-specific laws.
- Types of Acceptable Electronic Signatures: Specify which types of electronic signatures are recognized as valid within the organization (e.g., click-to-sign, graphical representations, biometric, digital certificates). Detail the security and authentication requirements for each.
- User Responsibilities: Outline the responsibilities of signers, document creators, and system administrators. This includes safeguarding login credentials, verifying signer identity, ensuring data accuracy, and reporting security incidents.
- Security Requirements: Detail the technical and administrative safeguards in place to protect electronic signatures and signed documents. This covers encryption standards, access controls, data integrity measures, and secure storage protocols.
- Authentication and Non-Repudiation: Describe the methods used to authenticate the identity of the signer and ensure that a signer cannot later deny having signed a document. This often involves robust audit trails and unique identifier linking.
- Audit Trails and Record Keeping: Mandate the creation and maintenance of comprehensive audit trails for every electronic signature event, including the identity of the signer, date/time, IP address, and details of the transaction. Specify record retention periods.
- Document Integrity and Archiving: Explain how the integrity of electronically signed documents will be maintained throughout their lifecycle, including secure archiving and retrieval processes.
- Training and Awareness: Outline requirements for mandatory training for all relevant personnel on the proper use of electronic signatures, the policy’s provisions, and security best practices.
- Non-Compliance and Sanctions: Clearly state the consequences for violating the policy, ranging from disciplinary action up to legal prosecution, emphasizing the seriousness of data security and compliance breaches.
- Policy Review and Updates: Establish a schedule for regular review and updates of the Electronic Signature Policy Template For Healthcare to ensure it remains current with technological advancements and regulatory changes.
Tips for Design, Usability, and Implementation
Successfully implementing an Electronic Signature Policy Template For Healthcare goes beyond simply drafting the document; it requires thoughtful design for usability and a strategic approach to implementation. The goal is to make the policy clear, actionable, and seamlessly integrated into daily operations.
For design and usability, focus on clarity and accessibility. The policy document itself should be easy to read and understand, avoiding overly technical jargon where simpler language suffices. Use clear headings, short paragraphs (as is done here), bullet points, and an intuitive structure. Consider providing a concise executive summary for busy stakeholders and detailed appendices for technical or legal specifics. Ensure the document is readily accessible, whether through an internal intranet, an HR portal, or as part of a compliance training module. Its design should encourage regular reference, not just a one-time read.
Regarding implementation, a phased approach often yields the best results. Instead of a "big bang" rollout, consider piloting the electronic signature process and the corresponding policy in a single department or for specific document types (e.g., administrative HR policies) before expanding. This allows for feedback gathering, process refinement, and training adjustments before a wider deployment. Provide comprehensive training to all affected staff, explaining not just how to use the technology, but why the policy and its security protocols are crucial for patient privacy and organizational compliance.
For digital implementation, integrate the electronic signature solution and its policy framework directly into existing workflows and systems, such as your Electronic Health Records (EHR) system, practice management software, or secure communication platforms. This minimizes disruption and enhances user adoption. Ensure that the chosen e-signature solution meets all technical requirements outlined in your Electronic Signature Policy Template For Healthcare, particularly concerning authentication, audit trails, and data security. Regularly audit the usage and compliance with the policy to identify any gaps or areas for improvement. While the policy primarily governs digital processes, having a print-friendly version of the policy document itself can be useful for training, reference materials, or situations where a physical copy is preferred by some users.
Embracing an Electronic Signature Policy Template For Healthcare is a pivotal step towards modernizing operations, enhancing data security, and ensuring legal compliance within your organization. It’s not merely a document but a strategic asset that guides the secure and efficient use of digital signatures across all facets of healthcare delivery. By leveraging such a template, you establish a clear, consistent framework that protects patient privacy, streamlines administrative tasks, and empowers your staff with the tools they need to operate effectively in a digital-first environment.
Investing the time and resources into customizing and implementing a robust Electronic Signature Policy Template For Healthcare will yield significant returns in terms of efficiency, risk mitigation, and confidence in your digital processes. It represents a commitment to best practices, demonstrating to patients, staff, and regulators alike that your organization prioritizes security, compliance, and innovation. Don’t just adopt technology; govern its use wisely with a policy that sets the standard for digital trust and accountability.